Genetics and Immune Disorders
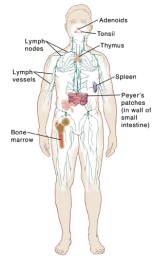
Your immune system is made up of a large network of cells, tissues, and organs. They work together to fight off infections and other harmful substances.
But the immune system doesn’t always work the way it should.
Some disorders make the immune system unable to fight off infections. In other disorders, the immune system actually attacks the body’s cells or organs, as it would attack an infection. This is what happens in autoimmune disorders, such as lupus and rheumatoid arthritis.
Immune disorders and genes
Genes are the building blocks of human growth and development. They control many features, such as hair and eye color. Genes also affect the way the immune system works or how it responds to threats. Primary immunodeficiency disorders are present at birth. They are often inherited. This means they are linked to genes passed from one generation to another. Some immune disorders are diagnosed at or shortly after birth. Other immune disorders may not have symptoms. Or they may not be diagnosed until later in childhood or adulthood.
Researchers keep learning how genes affect immune disorders. For example, one genetic defect may block certain cells defending the body. Another defect might stop the removal of toxic chemicals from the body.
Some symptoms of immune disorders
Symptoms of an immune disorder include:
-
Autoimmune disease symptoms, such as aching joints, tissue destruction, and inflammation
-
Trouble fighting infections or having infections that last a long time. For example:
-
Taking antibiotics for more than 1 or 2 months with no success
-
Having infections that other people fight off easily, such as fungal infections of the mouth or skin
-
-
Frequent, severe infections. For example, someone with a primary immune deficiency may have:
-
Many ear infections in a year
-
More than 1 lung, sinus, blood, bone, or deep skin infection in a year
-
-
Trouble growing or gaining weight as an infant
Complications
Complications of primary immune deficiency and genetic immune disorders include:
-
Death
-
Delayed development
-
Long-term or severe infections
Diagnosis
To diagnose genetic immune disorders, your healthcare providers may do some or all of the following:
-
Check your response to certain vaccines, such as tetanus or pneumococcal (pneumonia) vaccines
-
Order blood tests, including tests of antibody (immunoglobulin) levels, specialized tests of your white blood cells, or genetic testing
-
Review your personal and family health history
Treatment
Treatment may include:
-
Preventing infection. People who have immune disorders must work hard to not get an infection. Basic hygiene is very important. This includes handwashing. But it is also important not to be around crowds or people who have colds and illnesses. Children with specific immune disorders should not get live virus vaccines. This can cause sickness.
-
Long-term follow-up. Immune disorders mean an ongoing risk of infection. Work with your healthcare team to keep you as healthy as possible.
-
Treating existing infections. Antibiotics or antifungal treatments may be needed to treat the current infection. With severe infections, hospitalization may be needed.
-
Treating the immune deficiency. Treatment depends on the immune disorder. Treatments may include bone marrow transplants, and enzyme or antibody replacement therapy.